Issue Overview
Access to contraception is fundamental to reproductive autonomy and economic mobility for parents and their children. However, substantial upfront out-of-pocket costs for contraception severely limit access for those without health insurance. Though the Affordable Care Act (ACA) eliminated cost-sharing for contraception for those with health insurance, substantial cost-sharing remains for uninsured individuals who seek care through Title X: a national family planning program that offers subsidized, patient-centered reproductive health services for low-income individuals.
Bailey proposes two changes to Title X to make access to the contraception of choice more affordable:
- Make contraceptives free for low-income women through a change to the guidelines issued by the Department of Health and Human Services that defines the schedule of discounts; and,
- Increase congressional appropriations for the Title X program to fund this change in guidelines.
Similar to the ACA’s elimination of cost-sharing for contraception for Americans with health insurance, this proposal eliminates cost-sharing requirements for contraception for uninsured, low-income Americans through the Title X program.
This policy proposal is supported by direct evidence from a randomized control trial (RCT), described below. Eliminating cost-sharing for contraception through Title X would increase women’s ability to use their preferred contraceptive methods, reduce those pregnancies that they desire to delay or avoid, and generate substantial savings in government spending that could finance the program.
The Challenge
Inequities in access to contraception and reproductive health care have been well documented in the United States. In 2015, around 40% of pregnancies in the U.S. occurred either sooner than planned or when no pregnancy was desired. Inconsistent use or non-use of contraceptives is the most important proximate cause of unintended pregnancy. Over 95% of unintended pregnancies are driven by the 32% of women who use contraceptives inconsistently or not at all.
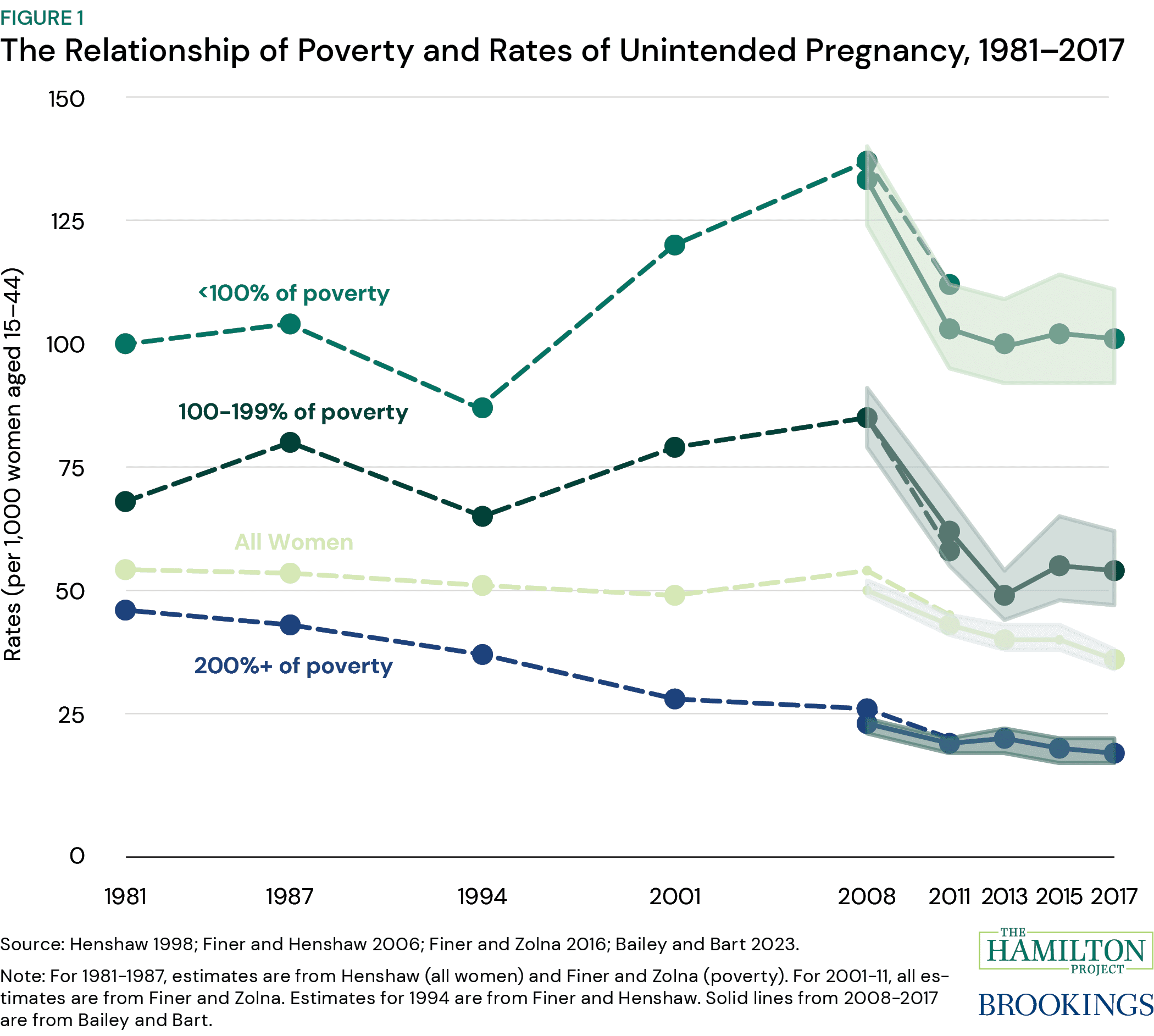
Mistimed or undesired pregnancies are five times more likely to occur among low-income women and are also more common among young and minority women. Considerable research documents the relationship between mistimed and undesired pregnancies and immediate adverse outcomes for mothers and their babies, including low infant birth weight, premature birth, and maternal morbidity and mortality. In the long-term, research documents how increasing access to contraception can facilitate women’s education and career advancement and improve the living circumstances of children.
In 2018, around 1.6 million Title X clients (or 40% of the total) were uninsured and faced substantial out-of-pocket costs for contraceptives after applying the Title X discounts. These costs are paid upfront. Prohibitively high costs for contraception present difficult choices for many low-income Americans: pay for housing and groceries this month and chance unplanned pregnancy or use a preferred method of contraception. Given these choices, it is not surprising that too few low-income, uninsured individuals use their preferred contraceptives.
About two in five mistimed or undesired pregnancies end in abortion. This means that the U.S. Supreme Court’s 2022 decision, Dobbs v. Jackson Women’s Health Organization, which has allowed states to restrict abortion access, is expected to increase the number of mistimed or undesired pregnancies resulting in childbirth in the U.S. to levels not seen since the 1990s (see figure 1).
The Proposal
Bailey proposes two changes to Title X to make access to the contraception of choice more affordable for those without health insurance:
- Make contraceptives free for low-income women through a change to the guidelines issued by the Department of Health and Human Services’ Office of Population Affairs by redefining the schedule of discounts to eliminate cost-sharing for contraceptives; and,
- Increase congressional appropriations for the Title X program to support the elimination of cost-sharing. Eliminating Title X cost-sharing for contraception would cost the federal government $178 million per year.
Eliminating cost-sharing for contraception through Title X would increase women’s ability to use their preferred contraceptive methods; reduce those pregnancies that they desire to delay or avoid, including those ending in both abortion and childbirth; and generate substantial savings in government spending that could effectively finance the program. These changes are expected to generate savings in government spending of $1.61 billion in the first year of the program, which could fund the expanded program for around four years. In addition to saving the federal government $804 million in the first year, states would save around $812 million combined.
The Michigan Contraceptive Access Research and Evaluation Study (M-CARES)
M-CARES is an RCT that evaluates how reduced cost-sharing at certain Title X clinics affects women’s ability to choose their preferred method of contraception and the subsequent effects of this increase in financial access on women’s life outcomes.
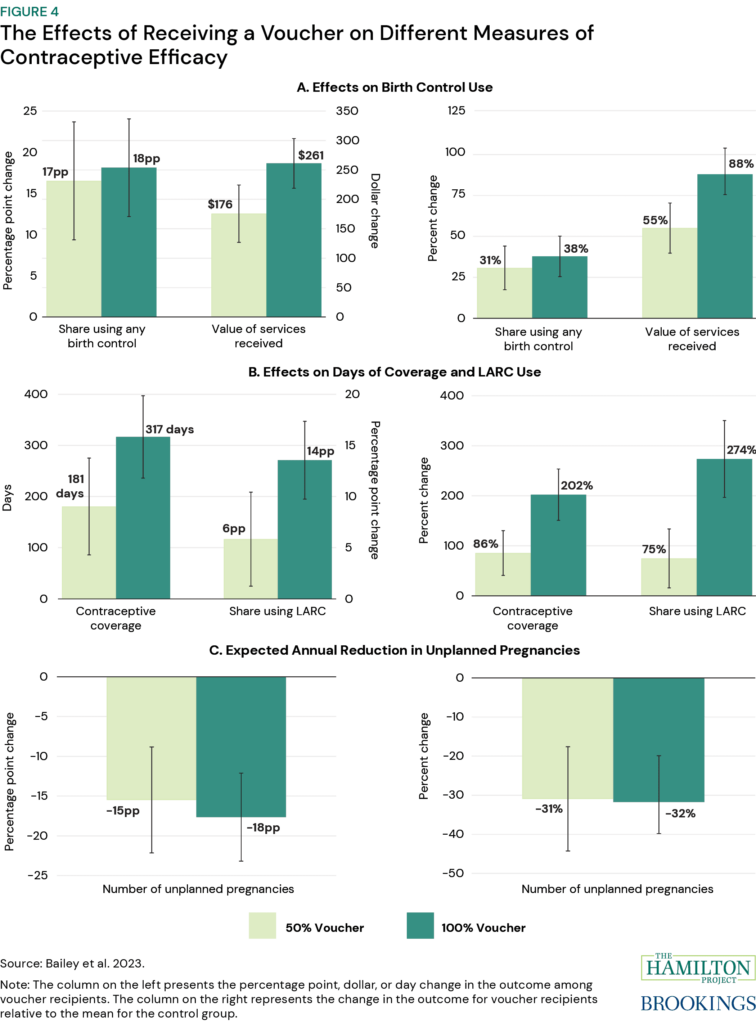
Between 2017 and 2023, this RCT removed or minimized cost as a barrier to choosing a preferred method of contraception. At random, participants were provided a voucher with a dollar value equivalent to either 50% or 100% of the total out-of-pocket costs for an uninsured woman to have an intrauterine device (IUD) inserted—one of the most expensive contraceptive options. This pricing scheme supported participants’ reproductive autonomy and eliminated cost barriers: the voucher makes any desired method of contraception financially accessible.
Bailey et al. (2023) find that both groups of voucher recipients were more likely to purchase contraceptives and spend more money on contraceptives. Even the reduced cost of contraception through the Title X sliding scale plays a significant role in limiting women’s choice of contraceptives: individuals who did not receive the voucher could not afford to purchase the contraceptives they desired. Eliminating cost-sharing allowed voucher recipients to purchase their preferred and typically more expensive and effective contraceptive methods and reduce the incidence of mistimed and undesired pregnancies.